Medical devices classified as Class IIb under Regulation (EU) 2017/745 (MDR) are considered medium-to-high risk and require a robust and proactive regulatory approach. These devices often interact more significantly with the human body than Class IIa devices and may support or monitor vital physiological processes. As such, they are subject to more stringent conformity assessment procedures, rigorous oversight by Notified Bodies, and comprehensive requirements for clinical evidence, risk management, and postmarket surveillance.
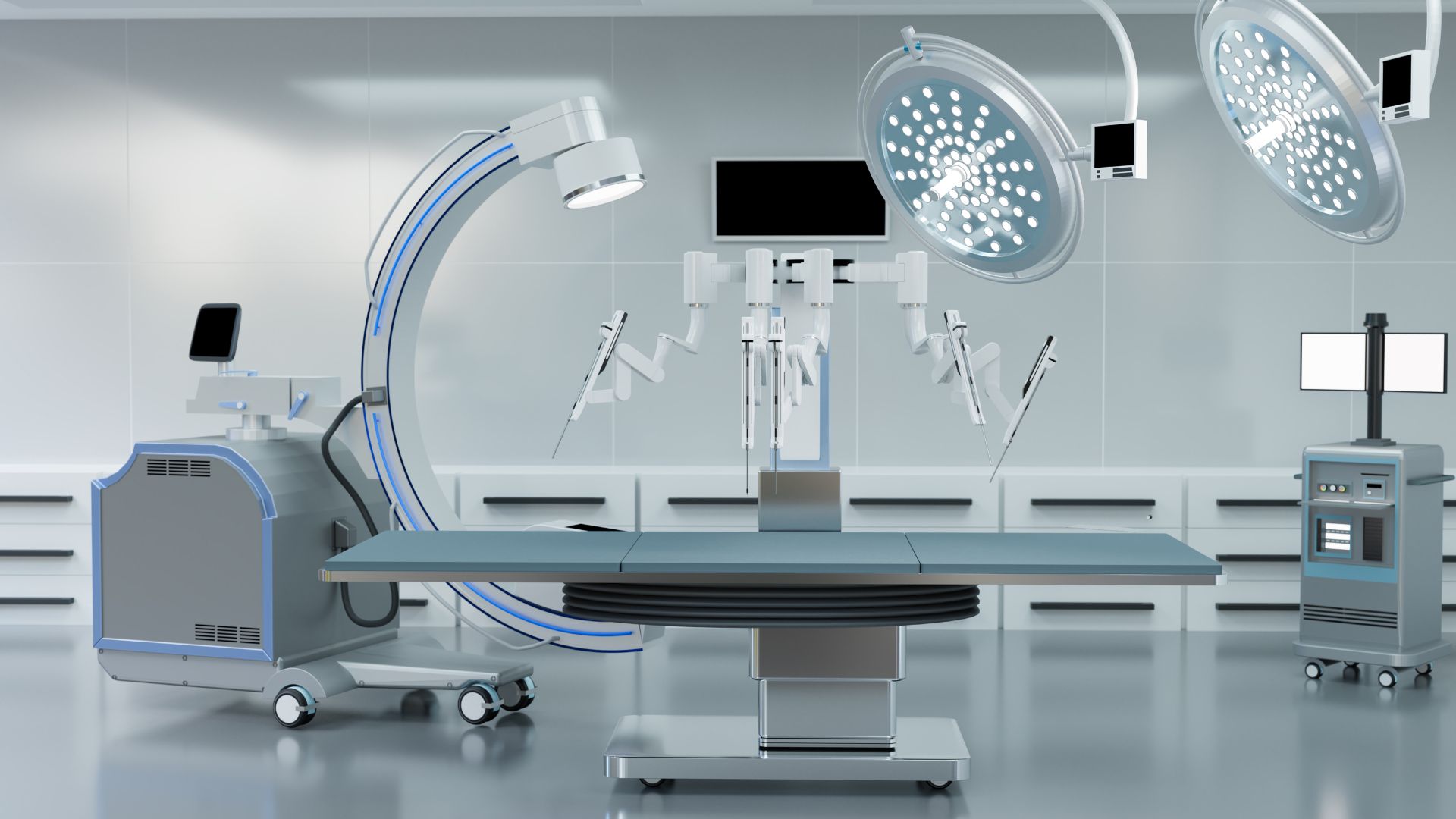
Typical Class IIb devices include anesthesia machines, infusion pumps with critical delivery functions, ventilators, surgical lasers, and diagnostic imaging systems that inform therapeutic decisions. They may be invasive, active, or used in critical care environments, necessitating both technical and procedural maturity to ensure regulatory compliance and clinical safety.
This article provides a detailed roadmap for Class IIb manufacturers—from classification criteria and conformity assessments to technical documentation, clinical evaluation, PMS, and economic operator responsibilities. For regulatory professionals and manufacturers looking to enter or expand in the EU market, understanding and executing a strategy for Class IIb compliance is a foundational requirement for long-term success.
Classification Criteria for EU Class IIb Devices
Classification under the MDR is based on a device’s intended use, duration of contact, invasiveness, and interaction with the human body. According to Annex VIII, Class IIb includes devices intended for:
- Long-term use in the central circulatory or central nervous system.
- Active delivery or removal of medicinal substances or energy with potentially hazardous effects.
- Life support, intensive care, or devices used for diagnostic or therapeutic monitoring in critical clinical contexts.
Rules frequently used to classify devices as Class IIb include Rules 8, 9, 10, 11, and 12. For example, Rule 10 applies to active therapeutic devices that administer or exchange energy to or from the patient, and depending on the level of energy or invasiveness, this can elevate a product from Class IIa to IIb.
Conformity Assessment Routes and Notified Body Involvement
Class IIb devices must undergo a conformity assessment involving a Notified Body. Manufacturers can follow:
- Annex IX (Full Quality Assurance): Involves assessment of the manufacturer’s entire QMS and selected technical documentation.
- Annex X (Type Examination): The Notified Body examines a representative sample and its documentation.
- Annex XI (Product Conformity Verification): A batch-by-batch conformity route, often used for high-variability or custom-made products.
Notified Bodies review the manufacturer’s clinical evidence, risk management documentation, PMS plans, and system controls. These interactions culminate in the issuance of a CE certificate, typically valid for five years but subject to annual surveillance and periodic recertification.
Unlike Class IIa, Class IIb devices are subject to greater scrutiny during both initial review and postmarket oversight. The Notified Body may require sampling across a wider range of technical files or more frequent PMS reviews.
Quality Management System and Risk Management Integration
The QMS must conform with MDR Article 10 and incorporate ISO 13485:2016 principles. It must demonstrate control over:
- Design and development (including design history files)
- Manufacturing processes (including process validation)
- Risk management integrated with ISO 14971 throughout the lifecycle
- Complaint handling and CAPA systems
- Supplier evaluation and auditing
- Software validation (if applicable)
The QMS must link all major compliance pillars—clinical evaluation, PMS, risk files, and technical documentation—so that any change in product design, performance data, or market behavior leads to timely updates and continuous improvement.
Clinical Evaluation and Evidence Requirements
Class IIb devices typically require significant clinical evidence. This includes both premarket and postmarket clinical data and must conform to Annex XIV of the MDR. The Clinical Evaluation Report (CER) must:
- Define the device’s intended purpose and claims
- Identify and justify equivalence (if applicable)
- Summarize relevant clinical literature, investigation results, and PMS/PMCF data
- Provide a risk-benefit assessment supported by clinical data
Notified Bodies assess the completeness, relevance, and robustness of the CER. Devices without a valid equivalence argument typically require new clinical investigations or PMCF studies. PMCF is not optional—it is expected to support continued clinical safety and performance.
Technical Documentation and Regulatory Submissions
Annex II and III describe the technical documentation requirements, including:
- Device description and specifications
- Manufacturing processes and quality controls
- Software architecture and validation
- Risk management reports and hazard traceability
- Labeling, IFU, and UDI information
- Summary of Safety and Clinical Performance (SSCP) for implantables and Class III-like functions
This documentation must be maintained throughout the product lifecycle and be readily available to regulators. Updates due to design changes, new clinical data, or adverse events must be reflected in the technical file in a timely and traceable manner.
Postmarket Surveillance and Vigilance
Manufacturers of Class IIb devices must implement a comprehensive PMS system, including:
- A device-specific PMS Plan (per Annex III)
- Periodic Safety Update Reports (PSUR) submitted annually
- PMCF Plans and Evaluation Reports
- Complaint trending, incident reporting, and signal detection processes
Under MDR Articles 87 to 89, serious incidents must be reported within specified timelines, and FSCAs must be supported by clear Field Safety Notices (FSNs). The PSUR must summarize clinical and PMS findings, volume of sales, and updates to the benefit-risk profile.
Authorized Representatives, Importers, and Distributors
Manufacturers outside the EU must appoint an Authorized Representative based within the EEA. This entity must have access to technical documentation and be named on product labeling and in EUDAMED.
Importers must verify CE marking, UDI, and compliance with labeling requirements. Distributors are responsible for maintaining storage conditions and reporting complaints. Agreements with these economic operators should define roles, vigilance reporting processes, and recall responsibilities.
UDI, EUDAMED Registration, and Labeling Compliance
Class IIb devices must be registered in EUDAMED and assigned a Basic UDI-DI and UDI-DI. Labels must include UDI in human- and machine-readable formats and reflect the device’s intended use, storage conditions, and regulatory markings.
The Summary of Safety and Clinical Performance (SSCP) must be available for devices that are implantable or perform life-sustaining functions. This document is published in EUDAMED and must be updated regularly.
Market Strategy and Long-Term Compliance
Regulatory compliance should not be separated from business planning. Class IIb devices often support critical therapies or diagnostics and may be subject to national tendering processes, public scrutiny, and academic evaluation.
Successful manufacturers align regulatory strategy with product development, sales, and lifecycle management. This includes horizon scanning for guidance updates, managing CER revisions, and investing in cross-functional training for regulatory, engineering, and commercial teams.
Market entry should be viewed as the beginning—not the end—of the regulatory journey. PMS, design evolution, and user feedback must inform future versions, new indications, and real-world performance claims.
Class IIb as a Pivotal Compliance Milestone
For many manufacturers, Class IIb represents the first regulatory threshold beyond moderate oversight. It requires commitment to transparency, operational maturity, and a culture of quality.
Mastering Class IIb compliance creates lasting value—not only in the form of CE marking, but through improved processes, validated claims, and defensible market presence. As MDR continues to evolve, companies that embed compliance into their core business functions will be positioned not just to survive audits—but to lead in patient safety, performance innovation, and regulatory confidence.